The Organisation for Economic Co-operation and Development (OECD) is an international organisation that regularly publishes its recommendations, analysis and data to help inform policy makers implement the best possible responses in their countries. In this article, Dr Merran Cooper summarises the key findings from a recent OECD report addressing end-of-life care.
With an ageing population bringing with it a higher number of chronic conditions, a growing share of the population will need end-of-life care. While end-of-life care services help improve quality of life through relieving pain and other symptoms, currently there are substantial gaps in the provision of services.
According to a report by the OECD, Time for Better Care at the End of Life (February 2023), end-of-life care does not always reflect the wishes of the patient and across OECD countries, hospitals are the predominant place of death, accounting for more than 50% of deaths.
Key findings of the report are that:
- Too many people receive sub-par care in their last days or months of life. Access to services is often insufficient and unequal, especially at home.
- Professionals often fail to discuss choices that provide people with a dignified end of life, and their care preferences are rarely recorded.
- Care provided at the end of life often fails to alleviate people-suffering and limit unnecessary treatments.
- Costs at the end of life are high for both the public purse and families, while not necessarily delivering quality of life, and there are questions about which different care models could improve outcomes for patients while reducing costs.
- Putting end-of-life care higher in the policy agenda and implementing a more comprehensive set of policies would make the end of life a more meaningful and humane experience for people and their relatives, and improve the outcomes achieved for the resources invested.
- The report emphasised the need for policy changes worldwide to improve the care people receive at the end of life and make care more person centred. These changes include recommendations for a range of measures and chief among them is facilitating patient consultation and respect for patient wishes.
Less than 50% of those aged over 65 had conversations about care choices
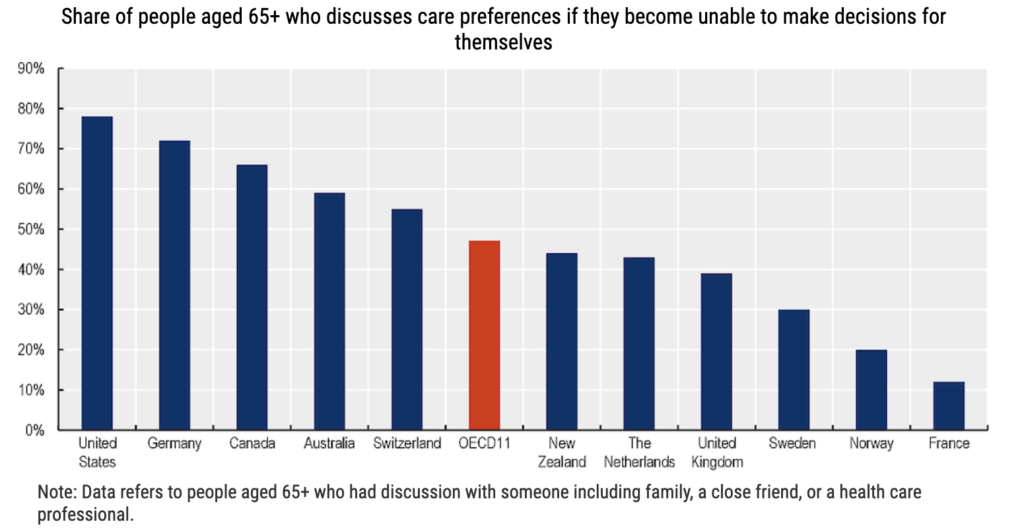
Recommendations include that decision making regarding the end of life should be inclusive, with people at the end of their life and their relatives able to plan care in advance to ensure that their preferences are clearly stated and taken into account. This would require improving awareness around care planning among the general population as well as professionals. Not planning care in advance might lead to undesired care and misalignment between preferences and experiences around the end of life (e.g. their preferred place of death). The lack of advance directives also puts the burden of choices on the patients’ relatives, who might not be aware of the patients’ preferences.
Australia is making strides with innovations such as Touchstone Life Care’s digital technology – providing an online solution to easily create and share advance care plans so care wishes are known. However, the report’s findings provide a wake-up call for all of us to do more to ensure that people receive the best possible care at the end of life. Let’s work together to make this a reality.

Dr Merran Cooper
Dr Merran Cooper MBBS. BSc (Physio), MAICD, M.Admin, PGD Adult Ed is a medical doctor and qualified physiotherapist. In 2018 she responded to the lack of good quality advance care planning in hospitals and the resultant overmedicalisation of dying by founding a technology company, Touchstone Life Care to develop an interoperable, real time advance care planning solution for consumers, providers and health systems.